The Science Behind Pelvic Floor Health: A Deep Dive
By ActiveCore Team | Date: October 26, 2023
The pelvic floor, often overlooked, is a crucial group of muscles and ligaments that form a sling-like structure at the base of the pelvis. These muscles play a vital role in supporting pelvic organs, maintaining continence, and contributing to sexual function. Understanding the intricate science behind pelvic floor health is the first step towards improving overall well-being and addressing common issues like incontinence or pelvic pain.
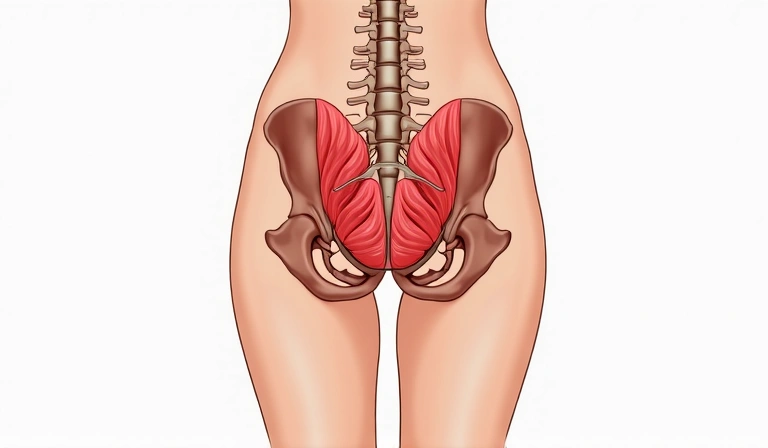
Comprising layers of muscles, fascia, and connective tissue, the pelvic floor acts as a dynamic hammock. Its primary functions include supporting the bladder, bowel, and uterus (in women), controlling the release of urine and feces, and enabling optimal sexual response. When these muscles are weak, overactive, or uncoordinated, a range of symptoms can arise, significantly impacting quality of life.

Anatomy and Function of the Pelvic Floor
The pelvic floor muscles are divided into superficial and deep layers. The superficial layer includes muscles like the bulbocavernosus, ischiocavernosus, and superficial transverse perineal muscles, which are involved in sexual function and support the perineum. The deep layer, primarily the levator ani and coccygeus muscles, provides the main support for the pelvic organs and plays a critical role in continence.
These muscles work in conjunction with the abdominal muscles, diaphragm, and deep back muscles to form the "core canister." This integrated system helps stabilize the spine and pelvis, manage intra-abdominal pressure, and facilitate efficient movement. Dysfunction in one part of this system can often lead to compensatory issues in another.
Common Pelvic Floor Dysfunctions
- Urinary Incontinence: This can range from stress incontinence (leakage with cough, sneeze, or laugh) to urge incontinence (sudden, strong need to urinate). Weak pelvic floor muscles are a common culprit, but hypertonic (overly tight) muscles can also contribute.
- Fecal Incontinence: Difficulty controlling bowel movements, often due to weakened or damaged anal sphincters and pelvic floor muscles.
- Pelvic Organ Prolapse: Occurs when pelvic organs (bladder, uterus, rectum) descend from their normal position and bulge into the vagina (in women) or rectum. This is typically due to stretched or weakened pelvic floor support structures.
- Pelvic Pain: Chronic pain in the pelvic region can be caused by various factors, including overactive, tight pelvic floor muscles (hypertonicity), nerve entrapment, or inflammation. Conditions like vaginismus, dyspareunia (painful intercourse), and chronic prostatitis are often linked to pelvic floor muscle dysfunction.
- Sexual Dysfunction: Both men and women can experience sexual difficulties related to the pelvic floor, including erectile dysfunction, painful intercourse, or difficulty achieving orgasm.
Causes and Risk Factors
Several factors can contribute to pelvic floor dysfunction:
Pregnancy and Childbirth: The physical stress of pregnancy and the trauma of vaginal delivery are significant risk factors for pelvic floor muscle weakness and damage. Hormonal changes during pregnancy also affect connective tissue elasticity.
Aging: As we age, muscle mass naturally decreases, and connective tissues may lose elasticity, leading to a decline in pelvic floor function. Menopause, with its associated hormonal shifts, can exacerbate these changes in women.
Chronic Strain: Conditions that cause chronic increased intra-abdominal pressure, such as chronic coughing (e.g., due to asthma or smoking), chronic constipation, or heavy lifting, can weaken the pelvic floor over time.
Obesity: Excess body weight places additional strain on the pelvic floor muscles and connective tissues, increasing the risk of prolapse and incontinence.
Surgery: Pelvic surgeries, such as hysterectomy or prostatectomy, can sometimes damage nerves or muscles of the pelvic floor, leading to dysfunction.
Neurological Conditions: Diseases affecting nerves, such as multiple sclerosis, Parkinson's disease, or spinal cord injuries, can impair pelvic floor muscle control.
Poor Posture and Movement Patterns: Suboptimal posture and dysfunctional movement patterns can impact the synergistic action of the core muscles, including the pelvic floor.
Treatment and Management
Fortunately, many pelvic floor dysfunctions can be effectively managed and improved with appropriate interventions. The approach often depends on the specific type and cause of the dysfunction.
Conservative Management
- Pelvic Floor Muscle Training (Kegel Exercises): Targeted exercises to strengthen, relax, or coordinate the pelvic floor muscles are often the first line of treatment. Proper technique is crucial; a pelvic floor physical therapist can provide guidance.
- Biofeedback: This technique uses sensors to provide real-time feedback on muscle activity, helping individuals learn to correctly identify and activate their pelvic floor muscles.
- Lifestyle Modifications: Addressing factors like chronic constipation (through diet and hydration), managing chronic cough, maintaining a healthy weight, and avoiding heavy lifting can significantly reduce strain on the pelvic floor.
- Bladder and Bowel Retraining: For incontinence issues, timed voiding schedules and strategies to suppress urgency can be highly effective.
- Dietary Changes: Certain foods and drinks (e.g., caffeine, artificial sweeteners, acidic foods) can irritate the bladder. Adjusting diet can help manage symptoms of overactive bladder.
Medical and Surgical Interventions
In some cases, especially for severe prolapse or incontinence that doesn't respond to conservative measures, medical or surgical interventions may be necessary. These can include medications, pessaries (support devices for prolapse), or various surgical procedures to repair damaged tissues or provide additional support.
The Role of a Pelvic Floor Physical Therapist
A specialized pelvic floor physical therapist is an invaluable resource for anyone experiencing pelvic floor dysfunction. These professionals have advanced training in assessing and treating conditions related to the pelvic floor. They can provide a comprehensive evaluation, identify the root cause of symptoms, and develop a personalized treatment plan that may include:
- Manual therapy techniques to release tight muscles or address scar tissue.
- Specific exercise prescriptions, often beyond basic Kegels, tailored to individual needs.
- Education on proper body mechanics, posture, and breathing techniques.
- Guidance on lifestyle modifications and self-management strategies.
- Modalities like electrical stimulation or cold laser therapy in some cases.
Empowering individuals with knowledge about their pelvic floor and providing them with the tools to manage their symptoms is central to improving long-term health and quality of life. Don't hesitate to seek professional help if you suspect you have pelvic floor dysfunction.